RESEARCH PAPER
Epidemiology of neurological disorders in Warangal, India – risk factor assessment-based prospective observational study
1
St. Peter’s Institute of Pharmaceutical Sciences, Hanumakonda, India
2
Rohini Super Specialty Hospital, India
3
Sri Sri Neuro Centre, India
Corresponding author
Rajasekhar Reddy Poonuru
St. Peter's Institute of Pharmaceutical Sciences, Vidyanagar,, 506001, Hanumakonda, India
St. Peter's Institute of Pharmaceutical Sciences, Vidyanagar,, 506001, Hanumakonda, India
Med Srod. 2023;26(3-4):49-52
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Neurological disorders are without a doubt among the most terrifying ailments that humans can experience. Although several observational studies on neurological illnesses have been conducted worldwide, there are relatively few such studies in India. The aim of the study is to research patients with neurological disorders in terms of their profiles, demographic data, family history, dietary habits, social habits, occupational status, geographical location, diagnosis, and treatment plan.
Material and methods:
The 6-month prospective observational study involved an in-depth interview schedule, and an information sheet in English and local languages using1,000 patients.
Results:
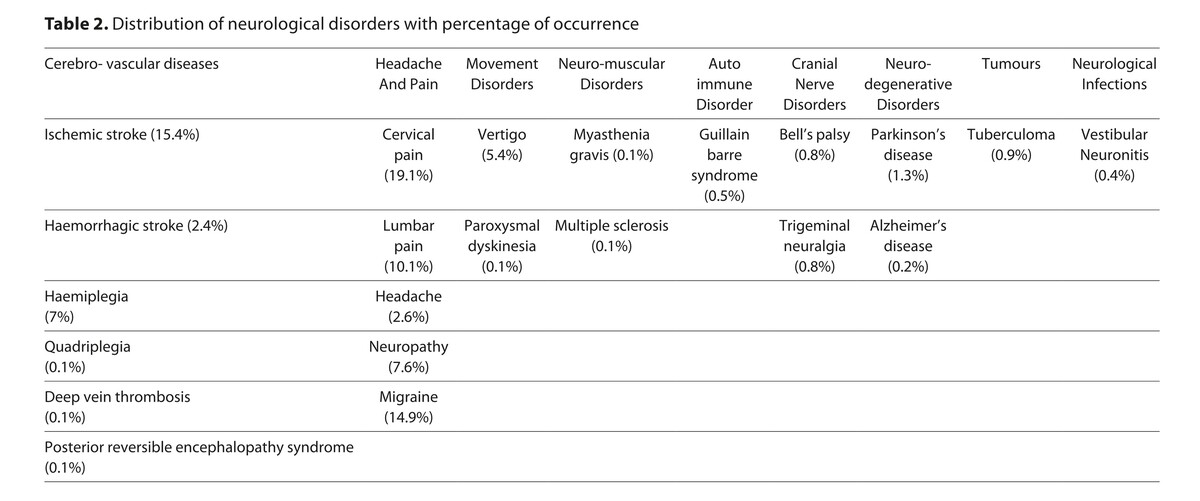
The findings of this study demonstrate that the prevalence of cervical discomfort followed by ischemic stroke is rather significant, and that neurological diseases were more common in rural areas than in metropolitan areas. Patients had hypertension (HTN), diabetes mellitus (DM), either alone or both together, Ischemic stroke, pain, epilepsy, thyroid, migraine, tuberculoma, and hamorrhagic stroke as previous illnesses.
Conclusions:
The prevalence of neurological problems was found to be higher in individuals over the age of 40 than in younger people. According to the statistics, females (58.5%) are more prone to neurological problems than males (41.5%). The patients’ body weight was also taken into account, and it was shown that the majority of the individuals with neurological diseases (33.7%) were of normal body weight. The frequency of neurological diseases was found to be much higher (55%) in rural regions than in urban areas (45%). The majority of patients with neurological illnesses were housewives. Analysis concluded that cervical discomfort is the most common neurological illness, compared to other neurological disorders.
Neurological disorders are without a doubt among the most terrifying ailments that humans can experience. Although several observational studies on neurological illnesses have been conducted worldwide, there are relatively few such studies in India. The aim of the study is to research patients with neurological disorders in terms of their profiles, demographic data, family history, dietary habits, social habits, occupational status, geographical location, diagnosis, and treatment plan.
Material and methods:
The 6-month prospective observational study involved an in-depth interview schedule, and an information sheet in English and local languages using1,000 patients.
Results:
The findings of this study demonstrate that the prevalence of cervical discomfort followed by ischemic stroke is rather significant, and that neurological diseases were more common in rural areas than in metropolitan areas. Patients had hypertension (HTN), diabetes mellitus (DM), either alone or both together, Ischemic stroke, pain, epilepsy, thyroid, migraine, tuberculoma, and hamorrhagic stroke as previous illnesses.
Conclusions:
The prevalence of neurological problems was found to be higher in individuals over the age of 40 than in younger people. According to the statistics, females (58.5%) are more prone to neurological problems than males (41.5%). The patients’ body weight was also taken into account, and it was shown that the majority of the individuals with neurological diseases (33.7%) were of normal body weight. The frequency of neurological diseases was found to be much higher (55%) in rural regions than in urban areas (45%). The majority of patients with neurological illnesses were housewives. Analysis concluded that cervical discomfort is the most common neurological illness, compared to other neurological disorders.
REFERENCES (38)
1.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. https://doi.org/10.1016/S0140-....
2.
Gourie-Devi M. Epidemiology of neurological disorders in India: review of background, prevalence and incidence of epilepsy, stroke, Parkinson's disease and tremors. Neurol India. 2014;62(6):588–598. https://doi.org/10.4103/0028-3....
3.
India State-Level Disease Burden Initiative Neurological Disorders Collaborators. The burden of neurological disorders across the states of India: The Global Burden of Disease Study 1990–2019. Lancet Glob Health. 2021;9(8):e1129-e1144. https://doi.org/10.1016/S2214-... (21)00164-9.
4.
GBD 2016 Parkinson's Disease Collaborators. Global, regional, and national burden of Parkinson's disease, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):939–953. https://doi.org/10.1016/S1474-....
5.
Mentis AFA, Dardiotis E, Efthymiou V, et al. non-genetic risk and protective factors and biomarkers for neurological disorders: a meta-umbrella systematic review of umbrella reviews. BMC Med. 2021;19:6. https://doi.org/10.1186/s12916....
6.
Government of India. Health benefit packages and empanelment criteria for Ayushman Bharat National Health Protection Scheme. 2018. https://pmjay.gov.in/sites/def... (accessed June 1, 2021).
7.
Man Mohan M, Vasundhara A. Neurological disorders in India: past, present, and next steps. 2021; 9:e1043–e1044. https://doi.org/10.1016/ S2214-109X(21)00214-X.
8.
GBD 2017 US Neurological Disorders Collaborators. Burden of Neurological Disorders Across the US From 1990–2017. A Global Burden of Disease Study. JAMA Neurol. 2021;78(2):165–176. https://doi.org/10.1001/jamane....
9.
Benjamin EJ, Virani SS, Callaway CW, et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67-e492. https://doi.org/10.1161/CIR.00....
10.
Hachinski V, Einhäupl K, Ganten D, et al. Preventing dementia by preventing stroke: the erlin manifesto. Alzheimers Dement. 2019;15(7):961–984. https://doi.org/10.1016/j.jalz....
11.
David Batty G, Philipp F, Urho MK, Seppo JS. Carlos AVH, Jaakko K. eClin Med. 2023;61:102056. https://doi.org/10.1016/j.ecli....
12.
Yerim K, Jee-Eun K, Sang-Hwa L, Dae YY, Jong SB. Analysis of Altmetrics in Social Recognition of Neurology and Neurological Disorders. Healthcare. 2020;8:367. https://doi.org/10.3390/health....
13.
Graff-Radford J, Simino J, Kantarci K, Mosley TH, Griswold ME, Windham BG, Sharrett AR, Albert MS, Gottesman RF, Jack CR, et al. Neuroimaging correlates of cerebral microbleeds: The ARIC Study (Atherosclerosis Risk in Communities). Stroke. 2017;48:2964–2972. https://doi.org/10.1161/STROKE....
14.
Hamilton OKL, Backhouse EV, Janssen E, Jochems ACC, Maher C, Ritakari TE, Stevenson AJ, Xia L, Deary IJ, Wardlaw JM. Cognitive impairment in sporadic cerebral small vessel disease: a systematic review and meta-analysis. Alzheimers Dement. 2021;17:665–685. https://doi.org/10.1002/alz.12....
15.
Iadecola C, Gottesman RF. Neurovascular and cognitive dysfunction in hypertension.Circ Res. 2019;124:1025–1044. https://doi.org/10.1161/CIRCRE....
16.
Conner SC, Pase MP, Carneiro H, Raman MR, McKee AC, Alvarez VE, Walker JM, Satizabal CL, Himali JJ, Stein TD, et al. Mid-life and late-life vascular risk factor burden and neuropathology in old age. Ann Clin Transl Neurol. 2019;6:2403–2412. https://doi.org/10.1002/acn3.5....
17.
Lane CA, Barnes J, Nicholas JM, Sudre CH, Cash DM, Malone IB, Parker TD, Keshavan A, Buchanan SM, Keuss SE, et al. Associations between vascular risk across adulthood and brain pathology in late life: evidence from a British Birth Cohort. JAMA Neurol. 2020;77:175–183. https://doi.org/10.1001/jamane....
18.
Boyle PA, Yu L, Wilson RS, Leurgans SE, Schneider JA, Bennett DA. Person-specific contribution of neuropathologies to cognitive loss in old age. Ann Neurol. 2018; 83:74–83. https://doi.org/10.1002/ana.25....
19.
Ding J, Davis-Plourde KL, Sedaghat S, Tully PJ, Wang W, Phillips C, Pase MP, Himali JJ, Gwen Windham B, Griswold M, et al. Antihypertensive medications and risk for incident dementia and Alzheimer’s disease: a meta-analysis of individual participant data from prospective cohort studies. Lancet Neurol. 2020;19:61–70. https://doi.org/10.1016/S1474-....
20.
van Middelaar T, Argillander TE, Schreuder FHBM, Deinum J, Richard E, Klijn CJM. Effect of antihypertensive medication on cerebral small vessel disease: a systematic review and meta-analysis. Stroke. 2018;49:1531–1533. https://doi.org/10.1161/STROKE....
21.
Williamson JD, Pajewski NM, Auchus AP, Bryan RN, Chelune G, Cheung AK, Cleveland ML, Coker LH, Crowe MG, Cushman WC, et al. Effect of intensive vs standard blood pressure control on probable dementia: A randomized clinical trial. JAMA. 2019;321:553561. https://doi.org/10.1001/jama.2....
22.
Mahinrad S, Kurian S, Garner CR, Sedaghat S, Nemeth AJ, Moscufo N, Higgins JP, Jacobs DR, Hausdorff JM, Lloyd-Jones DM, et al. Cumulative blood pressure exposure during young adulthood and mobility and cognitive function in midlife. Circulation. 2020;141:712–724. https://doi.org/10.1161/CIRCUL....
23.
El Tallawy HN, Farghaly WM, Rageh TA, Saleh AO, Mestekawy TA, Darwish MM, Abd El Hamed MA, Ali AM, Mahmoud DM. Construction of standardized Arabic questionnaires for screening neurological disorders (dementia, stroke, epilepsy, movement disorders, muscle and neuromuscular junction disorders). Neuropsychiatr Dis Treat. 2016;12:2245–2253. https://doi.org/10.2147/NDT.S1....
24.
Amr F, Ahmed S, Marwa F, Maged AN, Mohamed IH. Validation of cognitive screening questionnaire for neurological disorders (CSQND) for screening of cognitive complaints among patients with multiple sclerosis. Egypt J Neurol Psychiatry Neurosurg. 2022;58:98. https://doi.org/10.1186/s41983....
25.
GourieDevi M, Gururaj G, Satishchandra P. Neuroepidemiology in developing countries Manual for Descriptive Studies. National Institute of Mental Health and Neuro Sciences, Bangalore. (NIMHANS Publication No. 33) 1994;74.
26.
Gu Y, Beato JM, Amarante E, Chesebro AG, Manly JJ, Schupf N, Mayeux RP, Brickman AM. Assessment of Leisure time physical activity andbrain health in a multiethnic cohort of older adults. JAMA Netw Open. 2020;3:e2026506. https://doi.org/10.1001/jamane....
27.
Fouad A, Shawky A, Farghaly M. et al. Validation of cognitive screening questionnaire for neurological disorders (CSQND) for screening of cognitive complaints among patients with multiple sclerosis. Egypt J Neurol Psychiatry Neurosurg. 2022;58,98. https://doi.org/10.1186/s41983....
28.
Benedict RHB, Amato MP, DeLuca J, Geurts JJG. Cognitive impairment in multiple sclerosis: clinical management, MRI, and therapeutic avenues. Lancet Neurol. 2020;19(10):860–71. https://doi.org/10.1016/S1474-....
29.
Oliver SS, Ingrid H, Mark E, Markus R, Alan C, Jon S. Screening for functional neurological disorders by questionnaire. J Psychosom Res. 2019;119: 65–73. https://doi.org/10.1016/j.jpsy....
30.
Dehghani A. Development and validation of the disease – specific problems questionnaire for patients with multiple sclerosis. BMC Neurol. 2021;21:415. https://doi.org/10.1186/s12883....
31.
Moon H-J, Han S. Perspective: Present and Future of Virtual Reality for Neurological Disorders. Brain Sci. 2022;12(12):1692. https://doi.org/10.3390/brains....
32.
Chen Z, Rollo B, Baker A, et al. New era of personalised epilepsy management. BMJ2020;371:m3658. https://doi.org/10.1136/bmj.m3....
33.
Callixte KT, Tchaleu BC, Jacques D, Faustin Y, François DJ, Maturin TT. The pattern of neurological diseases in elderly people in outpatient consultations in Sub-Saharan Africa. BMC Res Notes. 2015;8:159–165.
34.
Gioffre-Florio M, Murabito LM, Visalli C, Pergolizzi FP, Fama F. Trauma in elderly patients: a study of prevalence, comorbidities and gender differences. G Chir. 2018;39(1):35–40. https://doi.org/10.11138/gchir....
35.
Stephen LJ, Harden C, Tomson T, Brodie MJ. Management of epilepsy in women. Lancet Neurol. 2019 May;18(5):481–491. https://doi.org/10.1016/S1474-....
36.
Panegyres PK, Gray V, Barrett L, Perceval S. Neurological disorders in a rural Western Australian population. Intern Med J. 2010:40(3):209–213. https://doi.org/10.1111/j.1445....
37.
Medawar E, Huhn S, Villringer A, et al. The effects of plant-based diets on the body and the brain: a systematic review. Transl Psychiatry. 2010;9:226. https://doi.org/10.1038/s41398....
38.
Pan B, Jin X, Jun L, Qiu S, Zheng Q, Pan M. The relationship between smoking and stroke: A meta-analysis. Medicine (Baltimore). 2019 Mar;98(12):e14872. https://doi.org/10.1097/MD.000....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.