Online first
Bieżący numer
O czasopiśmie
Archiwum
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Bazy indeksacyjne
Komitet Redakcyjny
Recenzenci
2024
2023
2022
2021
2020
2019
2018
Kontakt
Klauzula przetwarzania danych osobowych (RODO)
PRACA POGLĄDOWA
Jak zmniejszyć ryzyko zachorowania na raka jelita grubego? – przegląd czynników ryzyka związanych ze stylem życia
1
Student, Uniwersytet Medyczny w Lublinie, Polska
2
Kliniczny Oddział Toksykologiczno-Kardiologiczny i Chorób Wewnętrznych, Wojewódzki Szpital Specjalistyczny w Lublinie, Polska
3
Oddział Medycyny Paliatywnej, Samodzielny Publiczny Zakład Opieki Zdrowotnej w Łęcznej, Polska
Med Srod. 2025;28(1):29-33
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Rak jelita grubego jest jednym z najczęstszych nowotworów o niekorzystnym rokowaniu na świecie. Ryzyko zachorowania wydaje się być ściśle związane z czynnikami zewnętrznymi, na które człowiek narażony jest każdego dnia poprzez środowisko oraz styl życia. Praca przedstawia najważniejsze aspekty poruszone w wielu badaniach naukowych dotyczących rozwoju raka jelita grubego. Celem pracy jest analiza modyfikowalnych czynników ryzyka wystąpienia tego nowotworu oraz zwrócenie uwagi na możliwość zmniejszenia częstości występowania raka jelita grubego poprzez zmianę stylu życia.
Opis stanu wiedzy:
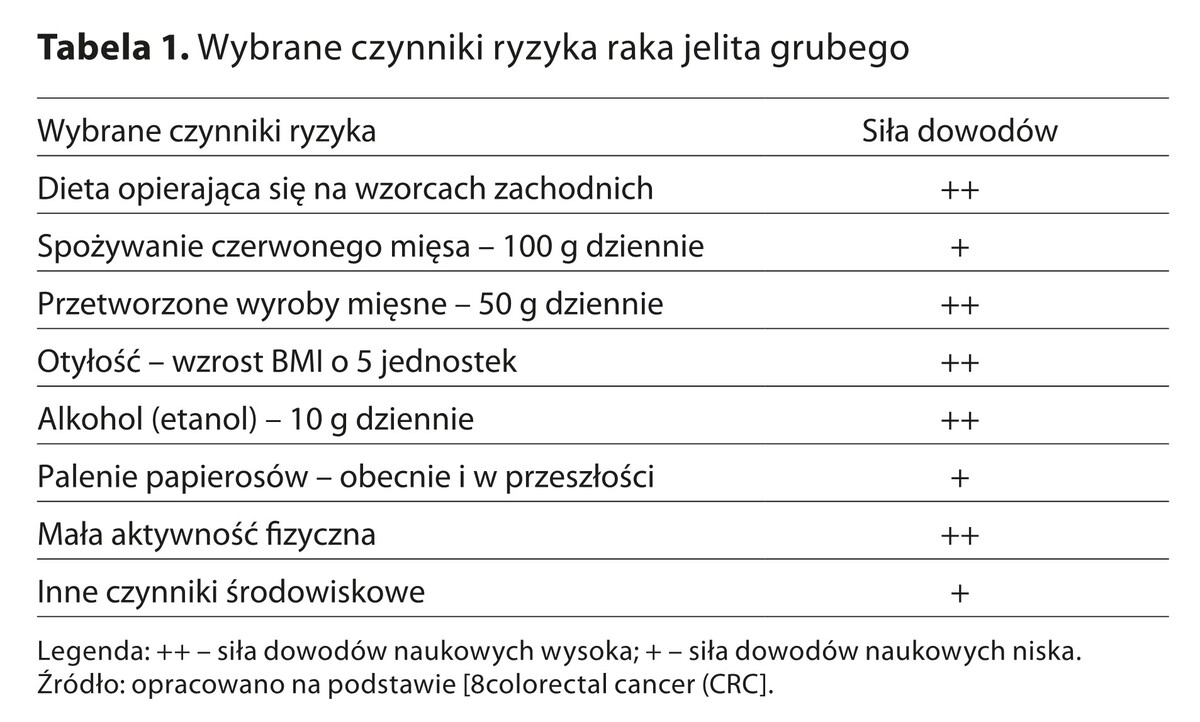
W ostatnich latach obserwuje się stopniowy wzrost liczby zachorowań na raka jelita grubego. Jest to nowotwór, który może wystąpić w każdym wieku. Proces nowotworzenia zostaje zainicjowany poprzez różne czynniki doprowadzające do powstania stanu zapalnego determinującego zwiększenie produkcji cytokin prozapalnych oraz hamującego mechanizmy obronne organizmu. Do najważniejszych czynników, które zwiększają ryzyko zachorowania na ten nowotwór, należy niewłaściwa dieta, otyłość oraz zaburzenia metaboliczne, palenie papierosów, mała aktywność fizyczna, a także narażenie na czynniki środowiskowe wpływające niekorzystnie na człowieka.
Podsumowanie:
Nieprawidłowa dieta, zaburzenia metaboliczne oraz gospodarki hormonalnej pacjentów przyczyniają się do powstania licznych miejscowych stanów zapalnych błony śluzowej jelit. Długotrwałe narażenie na zanieczyszczenia obecne w otoczeniu zwiększa ryzyko powstania komórek z nieprawidłowym DNA i procesów nowotworzenia. Rak jelita grubego jest ważnym problemem klinicznym na całym świecie, dlatego istotne jest podniesienie świadomości na temat czynników ryzyka oraz poprawa efektywności profilaktyki.
Rak jelita grubego jest jednym z najczęstszych nowotworów o niekorzystnym rokowaniu na świecie. Ryzyko zachorowania wydaje się być ściśle związane z czynnikami zewnętrznymi, na które człowiek narażony jest każdego dnia poprzez środowisko oraz styl życia. Praca przedstawia najważniejsze aspekty poruszone w wielu badaniach naukowych dotyczących rozwoju raka jelita grubego. Celem pracy jest analiza modyfikowalnych czynników ryzyka wystąpienia tego nowotworu oraz zwrócenie uwagi na możliwość zmniejszenia częstości występowania raka jelita grubego poprzez zmianę stylu życia.
Opis stanu wiedzy:
W ostatnich latach obserwuje się stopniowy wzrost liczby zachorowań na raka jelita grubego. Jest to nowotwór, który może wystąpić w każdym wieku. Proces nowotworzenia zostaje zainicjowany poprzez różne czynniki doprowadzające do powstania stanu zapalnego determinującego zwiększenie produkcji cytokin prozapalnych oraz hamującego mechanizmy obronne organizmu. Do najważniejszych czynników, które zwiększają ryzyko zachorowania na ten nowotwór, należy niewłaściwa dieta, otyłość oraz zaburzenia metaboliczne, palenie papierosów, mała aktywność fizyczna, a także narażenie na czynniki środowiskowe wpływające niekorzystnie na człowieka.
Podsumowanie:
Nieprawidłowa dieta, zaburzenia metaboliczne oraz gospodarki hormonalnej pacjentów przyczyniają się do powstania licznych miejscowych stanów zapalnych błony śluzowej jelit. Długotrwałe narażenie na zanieczyszczenia obecne w otoczeniu zwiększa ryzyko powstania komórek z nieprawidłowym DNA i procesów nowotworzenia. Rak jelita grubego jest ważnym problemem klinicznym na całym świecie, dlatego istotne jest podniesienie świadomości na temat czynników ryzyka oraz poprawa efektywności profilaktyki.
Introduction and objective:
Colorectal cancer is one of the most common cancers with a poor prognosis worldwide. The risk of the disease seems to be closely related to the external factors to which a person is exposed every day through the environment and lifestyle. The article presents the most important aspects discussed in many scientific studies on the development of colorectal cancer. The purpose of this study is to analyze modifiable risk factors for this cancer and to highlight the possibility of reducing the incidence of colorectal cancer through lifestyle changes.
Abbreviated description of the state of knowledge:
In recent years, there has been a gradual increase in the incidence of colorectal cancer. It is a neoplasm that can occur at any age. The process of carcinogenesis is initiated by various factors that lead to inflammation determining an increase in the production of pro-inflammatory cytokines and inhibiting the immune mechanisms. Among the most important factors that increase the risk of developing this cancer are unhealthy diet, obesity and metabolic disorders, smoking, low physical activity, as well as exposure to environmental factors that negatively affect a person.
Summary:
Unhealthy diet, metabolic and endocrine disorders of patients promote the development of multiple localized inflammations of the intestinal mucosa. Long-term exposure to pollutants present in the environment increases the risk of cells with abnormal DNA and tumorigenesis processes. Colorectal cancer is an important clinical problem occurring all over the world, so it is important to raise understanding of risk factors and improve the effectiveness of prevention.
Colorectal cancer is one of the most common cancers with a poor prognosis worldwide. The risk of the disease seems to be closely related to the external factors to which a person is exposed every day through the environment and lifestyle. The article presents the most important aspects discussed in many scientific studies on the development of colorectal cancer. The purpose of this study is to analyze modifiable risk factors for this cancer and to highlight the possibility of reducing the incidence of colorectal cancer through lifestyle changes.
Abbreviated description of the state of knowledge:
In recent years, there has been a gradual increase in the incidence of colorectal cancer. It is a neoplasm that can occur at any age. The process of carcinogenesis is initiated by various factors that lead to inflammation determining an increase in the production of pro-inflammatory cytokines and inhibiting the immune mechanisms. Among the most important factors that increase the risk of developing this cancer are unhealthy diet, obesity and metabolic disorders, smoking, low physical activity, as well as exposure to environmental factors that negatively affect a person.
Summary:
Unhealthy diet, metabolic and endocrine disorders of patients promote the development of multiple localized inflammations of the intestinal mucosa. Long-term exposure to pollutants present in the environment increases the risk of cells with abnormal DNA and tumorigenesis processes. Colorectal cancer is an important clinical problem occurring all over the world, so it is important to raise understanding of risk factors and improve the effectiveness of prevention.
REFERENCJE (34)
1.
O’Sullivan DE, Sutherland RL, Town S, et al. Risk Factors for Early-Onset Colorectal Cancer: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2022;20(6):1229–1240.e5. https://doi:10.1016/J.CGH.2021....
2.
Hua H, Jiang Q, Sun P, Xu X. Risk factors for early-onset colorectal cancer: systematic review and meta-analysis. Front Oncol. 2023;13. https://doi:10.3389/FONC.2023.....
3.
Schulpen M, van den Brandt PA. Mediterranean diet adherence and risk of colorectal cancer: the prospective Netherlands Cohort Study. Eur J Epidemiol. 2020;35(1):25–35. https://doi:10.1007/S10654–019....
4.
Bener A, Öztürk AE, Dasdelen MF, et al. Colorectal cancer and as-sociated genetic, lifestyle, cigarette, nargileh-hookah use and alcohol consumption risk factors: a comprehensive case-control study. Oncol Rev. 2024;18. https://doi:10.3389/OR.2024.14....
5.
Syed Soffian SS, Mohammed Nawi A, Hod R, et al. Meta-Analysis of the Association between Dietary Inflammatory Index (DII) and Colorectal Cancer. Nutrients. 2022;14(8). https://doi:10.3390/NU14081555.
6.
Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLO-BOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–249. https://doi:10.3322/CAAC.21660.
7.
AlZaabi A, Younus HA, Al-Reasi HA, Al-Hajri R. Could environmental exposure and climate change Be a key factor in the rising incidence of early onset colorectal cancer? Heliyon. 2024;10(16). https://doi:10.1016/J.HELIYON.....
8.
Keum NN, Giovannucci E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol. 2019;16(12):713–732. https://doi:10.1038/S41575–019....
9.
Zhong Y, Zhu Y, Li Q, et al. Association between Mediterranean diet adherence and colorectal cancer: a dose-response meta-analysis. Am J Clin Nutr. 2020;111(6):1214–1225. https://doi:10.1093/AJCN/NQAA0....
10.
Pacheco-Pérez LA, Ruíz-González KJ, De-La-Torre-Gómez AC, Guevara-Valtier MC, Rodríguez-Puente LA, Gutiérrez-Valverde JM. Environmental factors and awareness of colorectal cancer in people at familial risk. Rev Lat Am Enfermagem. 2019;27. https://doi:10.1590/1518–8345.....
11.
Lu L, Chen M, Zhang G, et al. Comprehensive profiling of extrachromosomal circular DNAs in colorectal cancer progression. Sci Rep. 2024;14(1). https://doi:10.1038/S41598–024....
12.
Agunwamba AA, Zhu X, Sauver JS, Thompson G, Helmueller L, Finney Rutten LJ. Barriers and facilitators of colorectal cancer screening using the 5As framework: A systematic review of US studies. Prev Med reports. 2023;35. https://doi:10.1016/J.PMEDR.20....
13.
Siegel RL, Jakubowski CD, Fedewa SA, Davis A, Azad NS. Colorectal Cancer in the Young: Epidemiology, Prevention, Management. Am Soc Clin Oncol Educ book Am Soc Clin Oncol Annu Meet. 2020;40(40):e75-e88. https://doi:10.1200/EDBK_27990....
14.
Lee SE, Jo HB, Kwack WG, Jeong YJ, Yoon YJ, Kang HW. Characteristics of and risk factors for colorectal neoplasms in young adults in a screening population. World J Gastroenterol. 2016;22(10):2981–2992. https://doi:10.3748/WJG.V22.I1....
15.
Hosseini FS, Nikparast A, Etesami E, Javaheri-Tafti F, Asghari G. The association between empirical dietary inflammatory pattern and risk of cancer and cancer-specific mortality: a systematic review and meta-analysis of prospective cohort studies. Front Nutr. 2024;11. https://doi:10.3389/FNUT.2024.....
16.
Li D, Hao X, Li J, et al. Dose-response relation between dietary inflammatory index and human cancer risk: evidence from 44 epidemiologic studies involving 1,082,092 participants. Am J Clin Nutr. 2018;107(3):371–388. https://doi:10.1093/AJCN/NQX06....
17.
Liu L, Tabung FK, Zhang X, et al. Diets That Promote Colon Inflammation Associate With Risk of Colorectal Carcinomas That Contain Fusobacterium nucleatum. Clin Gastroenterol Hepatol. 2018;16(10):1622–1631.e3. https://doi:10.1016/J.CGH.2018....
18.
Shivappa N, Godos J, Hébert JR, et al. Dietary Inflammatory Index and Colorectal Cancer Risk-A Meta-Analysis. Nutrients. 2017;9(9). https://doi:10.3390/NU9091043.
19.
Obón-Santacana M, Romaguera D, Gracia-Lavedan E, et al. Dietary Inflammatory Index, Dietary Non-Enzymatic Antioxidant Capacity, and Colorectal and Breast Cancer Risk (MCC-Spain Study). Nutrients. 2019;11(6). https://doi:10.3390/NU11061406.
20.
Alsheridah N, Akhtar S. Diet, obesity and colorectal carcinoma risk: results from a national cancer registry-based middle-eastern study. BMC Cancer. 2018;18(1). https://doi:10.1186/S12885–018....
21.
Gianfredi V, Salvatori T, Villarini M, Moretti M, Nucci D, Realdon S. Is dietary fibre truly protective against colon cancer? A systematic review and meta-analysis. Int J Food Sci Nutr. 2018;69(8):904–915. https://doi:10.1080/09637486.2....
22.
McNabb S, Harrison TA, Albanes D, et al. Meta-analysis of 16 studies of the association of alcohol with colorectal cancer. Int J Cancer. 2020;146(3):861–873. https://doi:10.1002/IJC.32377.
23.
Rawla P, Sunkara T, Barsouk A. Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol. 2019;14(2):89–103. https://doi:10.5114/PG.2018.81....
24.
Shen X, Wang Y, Zhao R, et al. Metabolic syndrome and the risk of colorectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis. 2021;36(10):2215–2225. https://doi:10.1007/S00384–021....
25.
Peruchet-Noray L, Sedlmeier AM, Dimou N, et al. Tissue-specific genetic variation suggests distinct molecular pathways between body shape phenotypes and colorectal cancer. Sci Adv. 2024;10(16). https://doi:10.1126/SCIADV.ADJ....
26.
Tian Y, Wang K, Li J, et al. The association between serum lipids and colorectal neoplasm: a systemic review and meta-analysis. Public Health Nutr. 2015;18(18):3355–3370. https://doi:10.1017/S136898001....
27.
Liu Y, Tang W, Wang J, et al. Association between statin use and colorectal cancer risk: a meta-analysis of 42 studies. Cancer Causes Control. 2014;25(2):237–249. https://doi:10.1007/S10552–013....
28.
Yang C, Wang X, Huang CH, Yuan WJ, Chen ZH. Passive Smoking and Risk of Colorectal Cancer: A Meta-analysis of Observational Studies. Asia-Pacific J public Heal. 2016;28(5):394–403. https://doi:10.1177/1010539516....
29.
Tomlinson MM, Pugh F, Nail AN, et al. Heavy-metal associated breast cancer and colorectal cancer hot spots and their demographic and socioeconomic characteristics. Cancer Causes Control. 2024;35(10). https://doi:10.1007/S10552–024....
30.
Jiang F, Zhao J, Sun J, et al. Impact of ambient air pollution on colorectal cancer risk and survival: insights from a prospective cohort and epigenetic Mendelian randomization study. EBioMedicine. 2024;103. https://doi:10.1016/J.EBIOM.20....
31.
Brynzak-Schreiber E, Schögl E, Bapp C, et al. Microplastics role in cell migration and distribution during cancer cell division. Chemosphere. 2024;353. https://doi:10.1016/J.CHEMOSPH....
32.
Dzierżyński E, Gawlik PJ, Puźniak D, et al. Microplastics in the Human Body: Exposure, Detection, and Risk of Carcinogenesis: A State-of-the-Art Review. Cancers (Basel). 2024;16(21). https://doi:10.3390/CANCERS162....
33.
Zhao J, Zhang H, Shi L, Jia Y, Sheng H. Detection and quantification of microplastics in various types of human tumor tissues. Ecotoxicol Environ Saf. 2024;283. https://doi:10.1016/J.ECOENV.2....
34.
Monteiro dos Santos JE, Campos Araújo M, Marcelo Furtado Passos da Silva C. Overweight is the main behavioral risk factor associated with colorectal cancer mortality in the Brazilian population: an ecological analysis. Sci Rep. 2024;14(1). https://doi:10.1038/S41598–024....
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.