RESEARCH PAPER
Potential impact of parents' lifestyle on the occurrence of leukemia in their children
1
Student Research Group, Department of Environmental Health, Faculty of Health Sciences in Bytom, Medical University
of Silesia, Katowice, Poland
2
Centre for Technology Transfer, Medical University of Silesia, Katowice, Poland
3
Department of Environmental Health, Faculty of Health Sciences in Bytom, Medical University of Silesia, Katowice,
Poland
Corresponding author
Małgorzata Ćwieląg-Drabek
Katedra Zdrowia Środowiskowego, Wydział Nauk o Zdrowiu w Bytomiu, Śląski Uniwersytet Medyczny w Katowicach, Polska, Piekarska 18, 41-902, Bytom, Polska
Katedra Zdrowia Środowiskowego, Wydział Nauk o Zdrowiu w Bytomiu, Śląski Uniwersytet Medyczny w Katowicach, Polska, Piekarska 18, 41-902, Bytom, Polska
Med Srod. 2020;23(1-4):18-25
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The most common cancers in children are leukemias, which account for approximately 25% of all cancers diagnosed in children in Poland. During 1999–2016, a total of 4,905 children and adolescents fell ill with leukemia, of whom 1,479 died. The study assumes that the exposure of parents in the pre-contraceptive period and the exposure of their children in the prenatal period to environmental carcinogens may influence the development of leukemia. Objective. The aim of this study was to analyze the occurrence of health risk factors in the families of children suffering from leukemia, caused by environmental pollution or the lifestyle of their parents.
Material and methods:
To achieve the assumed goal, a questionnaire study was conducted among 100 parents/legal guardians of children treated for leukemia.
Results:
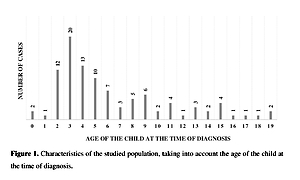
Statistical analyses of the data obtained showed a statistically significant correlation between the occurrence of leukemia in a child and: the child's age at diagnosis of the disease (p<.047), consumption of vegetables from their own cultivation by the respondents and their children (p<.048), and the use of plant protection products and artificial fertilizers in arable fields, allotment and home gardens owned by the respondents (p<.003).
Conclusions:
In order to reduce the health risk associated with the occurrence of neoplastic diseases of the blood in the population of children, actions should be taken to increase the awareness of the general population about the presence of carcinogenic and haematotoxic factors in the human living environment.
The most common cancers in children are leukemias, which account for approximately 25% of all cancers diagnosed in children in Poland. During 1999–2016, a total of 4,905 children and adolescents fell ill with leukemia, of whom 1,479 died. The study assumes that the exposure of parents in the pre-contraceptive period and the exposure of their children in the prenatal period to environmental carcinogens may influence the development of leukemia. Objective. The aim of this study was to analyze the occurrence of health risk factors in the families of children suffering from leukemia, caused by environmental pollution or the lifestyle of their parents.
Material and methods:
To achieve the assumed goal, a questionnaire study was conducted among 100 parents/legal guardians of children treated for leukemia.
Results:
Statistical analyses of the data obtained showed a statistically significant correlation between the occurrence of leukemia in a child and: the child's age at diagnosis of the disease (p<.047), consumption of vegetables from their own cultivation by the respondents and their children (p<.048), and the use of plant protection products and artificial fertilizers in arable fields, allotment and home gardens owned by the respondents (p<.003).
Conclusions:
In order to reduce the health risk associated with the occurrence of neoplastic diseases of the blood in the population of children, actions should be taken to increase the awareness of the general population about the presence of carcinogenic and haematotoxic factors in the human living environment.
FUNDING
Funding. The study was funded by the Medical University
of Silesia in Katowice, Poland (Grant No. KNW-1–094/
N/7/Z and KNW-1–99/N/9/Z).
REFERENCES (36)
1.
Kaatsch P. Epidemiology of childhood cancer. Cancer Treat Rev. 2010; 36(4): 277–285. doi: 10.1016/j.ctrv.2010.02.003.
2.
Szymborski J. Public health and population policy. Warsaw: Government Population Council; 2012. p. 40–64. [in Polish].
3.
National Center for Injury Prevention and Control. Ten Leading Causes of Death and Injury. 2016. https://www.cdc.gov/injury/wis.... [access: 20.10.2019].
4.
Steliarova-Foucher E, Colombet M, Ries LAG., et al. International incidence of childhood cancer, 2001–10: a population-based registry study. Lancet Oncol. 2017; 18(6): 719–731. doi: 10.1016/S1470–2045(17)30186-9.
5.
Szymborski J, Didkowska J, Wojciechowska U. Malignant neoplasms in children and adolescents in Poland. Incidence and mortality from malignant neoplasms and the demographic situation of Poland. Warsaw: Government Population Council; 2014. p. 117–146. [in Polish].
6.
Wojciechowska U, Didkowska J. Morbidity and mortality from malignant neoplasms in Poland. National Cancer Registry. Oncology Center – Institute of Maria Skłodowska-Curie. 2019. http://onkologia.org.pl/raport... [access: 09.10.2019].
7.
Gupta S, Howard S, Hunger S, et al. Treating Childhood Cancers in Low- and Middle-Income Countries. In: Cancer: Disease Control Priorities. Third edition (Volume 3). Washington (DC): The World Bank; 2015. http://dcp-3.org/chapter/900/t... [access: 09.10.2019].
8.
Israels T, Challinor J, Howard S, et al. Treating Children With Cancer Worldwide – Challenges and Interventions. Pediatrics 2015; 136(4): 607–610. doi: doi.org/10.1542/peds.2015-0300.
9.
Stewart BW, Wild CP, editor. World Cancer Report 2014. International Agency for Research on Cancer. Lyon: World Health Organization; 2014.
10.
Strumylaite L. Cancer risk in relations to exposure to trace elements. Environ Med. 2011; 14(1): 7–12.
11.
Commission for Environmental Cooperation. Toxic Chemicals and Children›s Health in North America. A Call for Efforts to Determine the Sources, Levels of Exposure, and Risks that Industrial Chemicals Pose to Children›s Health. CEC Project Report. 2006. http://www3.cec.org/islandora/... [access: 09.10.2019].
12.
Gouveia-Vigeant T, Tickner J. Toxic chemicals and childhood cancer: A review of the evidence. A Publication of the Lowell Center for Sustainable Production. University of Massachusetts Lowell. 2013. https://sustainableproduction…. [access: 09.10.2019].
13.
Norman RE, Ryan A, Grant K, et al. Environmental Contributions to Childhood Cancers. J Environ Immunol Toxicol. 2014; 1(4): 190–202. doi: 10.7178/jeit.17.
14.
Hunger SP, Mullighan CG. Acute Lymphoblastic Leukemia in Children. N Engl J Med. 2015; 373(16): 1541–1552. doi: 10.1056/NEJMra1400972.
15.
Jin MW, Xu SM, An Q, et al. A review of risk factors for childhood leukemia. Eur Rev Med Pharmacol Sci. 2016; 20(18): 3760–3764.
16.
Schmieglow K, Vestergaard T, Nielsen SM, et al. Etiology of common childhood acute lymphoblastic leukemia; the adrenal hypothesis. Leukemia 2008; 22: 2137–2141. doi: 10.1038/leu.2008.212.
17.
Ward MH, Colt JS, Metayer C, et al. Residential exposure to polychlorinated biphenyls and organochlorine pesticides and risk of childhood leukemia. Environ Health Perspect. 2009; 117(6): 1007–1013. doi: 10.1289/ehp.0900583.
18.
Chokkalingam AP, Bartley K, Wiemels JL, et al. Haplotypes of DNA repair and cell cycle control genes, x-ray exposure, and risk of childhood acute lymphoblastic leukemia. Cancer Causes Control 2011; 22(12): 1721–1730. doi: 10.1007/s10552-011-9848-y.
19.
Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012; 380(9840): 499–505. doi: 10.1016/S0140-6736(12)60815-0.
20.
Vinceti M, Rothman KJ, Crespi CM, et al. Leukemia risk in children exposed to benzene and PM10 from vehicular traffic: a case-control study in an Italian population. Eur J Epidemiol. 2012; 27(10): 781–790. doi: 10.1007/s10654-012-9727-1.
21.
Preston DL, Cullings H, Suyama A, et al. Solid cancer incidence in atomic bomb survivors exposed in utero or as young children. J Natl Cancer Inst. 2008; 100(6): 428–436. doi: 10.1093/jnci/djn045.
22.
Moore LE, Lu M, Smith AH. Childhood Cancer Incidence and Arsenic Exposure in Drinking Water in Nevada. Arch Environ Health An Int J. 2002; 57(3): 201–206. doi: 10.1080/00039890209602937.
23.
Sikorska-Jaroszyńska MHJ, Mielnik-Błaszczak M, Krawczyk D, et al. Passive smoking as an environmental health risk factor. Ann Agric Environ Med. 2012; 19(3): 547–550.
24.
Heck JE, Wu J, Lombardi C, et al. Childhood Cancer and Traffic-Related Air Pollution Exposure in Pregnancy and Early Life. Environ Health Perspect. 2013; 121(11–12): 1385–1391. doi: 10.1289/ehp.1306761.
25.
Deziel NC, Rull RP, Colt JS, et al. Polycyclic Aromatic Hydrocarbons in Residential Dust and Risk of Childhood Acute Lymphoblastic Leukemia. Environ Res. 2014; 133: 388–395. doi: 10.1016/j.envres.2014.04.033.
26.
Malagoli C, Malavolti M, Costanzini S, et al. Increased incidence of childhood leukemia in urban areas: a population-based case-control study. Epidemiol Prev. 2015; 39(4 Suppl 1): 102–107.
27.
Rumrich IK, Viluksela M, Vahakangas K, et al. Maternal Smoking and the Risk of Cancer in Early Life – A Meta-Analysis. PLoS One. 2016; 11(11): e0165040. doi: 10.1371/journal.pone.0165040.
28.
D'andrea MA, Reddy GK. Health Risks Associated With Benzene Exposure in Children: A Systematic Review. Glob Pediatr Health. 2018; 5: 2333794X18789275. doi: 10.1177/2333794X18789275.
29.
Khani Y, Pourgholam-Amiji N, Afshar M, et al. Tobacco Smoking and Cancer Types: A Review. Biomedical Res Ther. 2018; 5(4): 2142–2159.
30.
Szymala I. The incidence of leukemia and malignant lymphoma in children in the Silesia Province in terms of environmental pollution. Dissertation. Medical University of Silesia in Katowice. Bytom, Poland. 2018.
31.
Carpenter DO, Bushkin-Bedient S. Exposure to chemicals and radiation during childhood and risk for cancer later in life. J Adol Health. 2013; 52(5): 21–29. doi: 10.1016/j.jadohealth.2013.01.027.
32.
Topiłko A, Radwańska U, et al. Morphological analysis and differential diagnosis of ac. leukemia in children by electron microscopy. J Submicroscop Cytology 1974; 6: 191.
33.
Radwańska U, Michalewska D, et al. The results of intensive treatment of 426 children with acute lymphoblastic leukemia. Acta Haemat Pol. 1981; 12: 175. [in Polish].
34.
International Agency for Research on Cancer. IARC Monographs on the Identification of Carcinogenic Hazards to Humans. Agents Classified by the IARC Monographs, 2019, Volumes 1–124. https://monographs.iarc.fr/age... [access: 10.09.2019].
35.
Ki-Hyun K, Kabir E, Jahan SA. Exposure to pesticides and the associated human health effects. Sci Total Environ. 2017; 575: 525–535. doi: 10.1016/j.scitotenv.2016.09.009.
36.
World Health Organization. WHO's Urban Ambient Air Pollution database Update. 2018. https://www.who.int/airpolluti... [access: 10.09.2019].
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.