REVIEW PAPER
Protothecosis in humans and animals
1
Uniwersytet Przyrodniczy w Lublinie, Polska
Corresponding author
Med Srod. 2021;24(1-4):18-24
KEYWORDS
TOPICS
Health effects of environmental pollutionEnvironmental toxicology (physical, chemical and biological factors)
ABSTRACT
Introduction and objective:
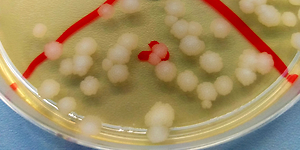
The algae from the Prototheca genus are very interesting and unique microorganisms belonging to the plant kingdom (Regnum Vegetabile), which are capable of infecting animals and humans, causing a disease called protothecosis. For a long time, algae of the genus Prototheca were not recognized as pathogens dangerous to humans. Possible isolations of these microorganisms from wounds, blood or faeces were usually interpreted as saprophytes or impurities. The objective of the study is presentation of the current state of knowledge concerning the biology, identification and pathogenicity for animals and humans caused by achlorophyllic algae of the genus Prototheca.
Brief description of the state of knowledge:
Protothecosis is a fairly rare infection caused by the achlorophyllic algae of the genus Prototheca, which are widespread in the environment. These algae are pathogens for animals and humans. Prototheca spp. may cause human infections, but they are also a problem in animal infections, mainly when it comes to mastitis in dairy cows, causing far-reaching economic losses. The structure of Prototheca algae makes them resistant to most fungistatics, antibiotics, and disinfectants, and is also resistant to high temperatures.
Summary:
Due to the capability of infecting animal and human organisms, and wide resistance to many factors and agents, it is important to deepen the knowledge concerning Prototheca algae and better recognize these extremely interesting microorganisms, in order to be able to cure protothecosis more effectively in the future. Considering an increasing number of people with reduced immunity this disease may affect an increasing number of humans; however, also animals.
The algae from the Prototheca genus are very interesting and unique microorganisms belonging to the plant kingdom (Regnum Vegetabile), which are capable of infecting animals and humans, causing a disease called protothecosis. For a long time, algae of the genus Prototheca were not recognized as pathogens dangerous to humans. Possible isolations of these microorganisms from wounds, blood or faeces were usually interpreted as saprophytes or impurities. The objective of the study is presentation of the current state of knowledge concerning the biology, identification and pathogenicity for animals and humans caused by achlorophyllic algae of the genus Prototheca.
Brief description of the state of knowledge:
Protothecosis is a fairly rare infection caused by the achlorophyllic algae of the genus Prototheca, which are widespread in the environment. These algae are pathogens for animals and humans. Prototheca spp. may cause human infections, but they are also a problem in animal infections, mainly when it comes to mastitis in dairy cows, causing far-reaching economic losses. The structure of Prototheca algae makes them resistant to most fungistatics, antibiotics, and disinfectants, and is also resistant to high temperatures.
Summary:
Due to the capability of infecting animal and human organisms, and wide resistance to many factors and agents, it is important to deepen the knowledge concerning Prototheca algae and better recognize these extremely interesting microorganisms, in order to be able to cure protothecosis more effectively in the future. Considering an increasing number of people with reduced immunity this disease may affect an increasing number of humans; however, also animals.
REFERENCES (48)
1.
Rudna J, Bakuła Z, Jagielski T. Występowanie glonów z rodzaju Prototheca w środowisku naturalnym. Post Mikrobiol. 2019; 58(1): 94.
2.
Moneta S, Bakuła Z, Jagielski T. Lekowrażliwość i typowanie genetyczne szczepów Prototheca spp. izolowanych z przypadków prototekozy u psów. Post Mikrobiol. 2019; 58(1): 102.
3.
Pal M, Abraha A, Rahman T Md, et al. Protothecosis: an emerging glonal disease of humans and animals. Int J Life Sci Biotech Pharm Res. 2014; 3(4): 1–13.
4.
Lass-Flör C, Mayr A. Human protothecosis. Clin Microbiol Rev. 2007; 20(2), 230–242.
5.
Hillesheim P B, Bahrami S. Cutaneous protothecosis. Arch Pathol Lab Med. 2011; 135: 941–944.
6.
Krukowski H. Zapalenia wymienia u krów wywołane przez grzyby i glony. cz.2. Prototekoza wymienia. Magazyn hodowcy 2014; 1: 22–27.
7.
Jagielski T, Karnkowska A, Bakuła Z, et al. The genus Prototheca (Trebouxiophyceae, Chlorophyta) revisited: Implications from molecular taxonomic studies. Glonal Res. 2019; 43: 101639.
8.
Milanov D, Petrović T, Polaček V, et al. Mastitis associated with Prototheca zopfii – an emerging health and economic problem on dairy farms. J Vet Res. 2016; 60: 373–378.
9.
Amhed F. Y, Application of phase-contrast microscope for detection of Prototheca spp. microalgae in tissue section-first record (Note). Egypt J Vet Sci. 2020; 51, 1: 89–91.
10.
Smulski S. Rzadko spotykane czynniki etiologiczne mastitis u krów. Weterynaria w terenie. 2018; 1: 52–56.
11.
Gregorczuk S, Bakuła Z, Krukowski H, et al. Nowa metoda identyfikacji Prototheca spp. wykorzystująca analizę PCR-RFLP genu 18S rDNA. Wydział Biologii Uniwersytet Warszawski, 2014.
12.
Roeske K, Dulko E, Jagielski T. Typowanie glonów Prototheca spp. techniką High Resolution Melting Real-Time PCR, Post Mikrobiol. 2019; 58, 1: 76.
13.
Zeng X, Kudinha T, Kong F, et al. Comparative genome and transcriptome study of the gene expression difference between pathogenic and environmental strains of Prototheca zopfii. Front Microbiol. 2019; 10, 443: 1–14.
14.
Murugaiyan J, Ahrholdt J, Kowbel V, et al. Establishment of a matrixassisted laser desorption ionization time-offlight mass spectrometry database for rapid identification of infectious achlorophyllous green micro-algae of the genus Prototheca. Clin Microbiol Infect. 2012; 18, 5: 461–467.
15.
Masuda M, Hirose N, Ishikawa T, et al. Prototheca miyajii sp. nov., isolated from a patient with systemic protothecosis. Int J Syst Evol Microbiol. 2016; 66: 1510–1520.
16.
Zhao F, Chen M, Fu Y. Multiple cutaneous infections caused by Prototheca wickerhamii. J Clin Lab Anal. 2020; 34(11): 1–4.
17.
Jagielski T, Gawor J, Bakuła Z, et al. cytb as a new genetic marker for differentiation of Prototheca species. J Clin Microbiol. 2018; 56(10): e00584–18.
18.
Solky A C, Laver N M, Williams J, et al. Prototheca wickerhamii infection of a corneal graft. Cornea. 2011; 30, 10: 1173–1175.
19.
Godofredo Romero V, Enokihara MM, Tomimori J, et al. Cutaneous protothecosis in kidney transplant recipient. An Bras Dermatol. 2020; 95(2): 210–213.
20.
Satoh K, Ooe K, Nagayama H, et al. Prototheca cutis sp. nov., a newly discovered pathogen of protothecosis isolated from inflamed human skin. Int J Syst Evol Microbiol. 2010; 60: 1236–1240.
21.
Minato K, Yoshikawa M, Nakanishi H, et al. Long Term Follow-Up of Prototheca keratitis. Int Medical Case Rep J. 2020; 13: 503–506.
22.
Seok J Y, Lee Y, Lee H, et al. Human Cutaneous Protothecosis: Report of a case and literature review. Korean J Pathol. 2013; 47: 575–578.
23.
Nguyen Ly Q G, Rosen T. Cutaneous protothecosis in a patient with chronic lymphocytic leukemia: A case report and literature review. J Fungi. 2015; 1: 4–12.
24.
Kazantseva IA, Molochkov AV, Sukhov AV, et al. A case of cutaneous protothecosis. Arkh Patol. 2017; 1: 52–55.
25.
Rajan A, Pai V V, Shukla P. Cutaneous protothecosis in an immunocompetent host. Indian J. Dermatol. Venereol Leprol. 2020; 86: 414–417.
26.
Yagnik K, Bossé R, Reppucci J, et al. Case Report: Olecranon bursitis due to Prototheca wickerhamii in an immunocompromised patient. Am J Trop Med Hyg. 2019; 100, 3: 703–705.
27.
Zhang Q Q, Zhu L P, Weng X H, et al. Meningitis due to Prototheca wickerhamii: rare case in China. Med Mycol. 2007; 45: 85–88.
28.
Żak I, Jagielski T, Kwiatkowski S, et al. Prototheca wickerhamii as a cause of neuroinfection in a child with congenital hydrocephalus.First case of human protothecosis in Poland. Diagn Microbiol Infect Dis. 2012; 74(2): 186–189.
29.
Yi Sim J. Fatal disseminated infection caused by Prototheca zopfii in a child with leukemia. J Microbiol Immunol Infect. 2019; 52: 833–835.
30.
Joerger T, Sulieman S, Carson VJ, et al. Chronic meningitis due to Prototheca zopfii in an adolescent girl. J Pediatric Infect Dis Soc. 2021; 10(3): 370–372.
31.
El Hoshy K, Abdel-Halim MRE, El Nabarawy E, et al. Cutaneous protothecosis as an unusual complication following dermal filler injection: A case report. J Clin Aesthet Dermatol. 2019; 12(12): 13–16.
32.
Jagielski T, Dyląg M, Roesler U, et al. Isolation of infectious microalga Prototheca wic-kerhamii from a carp (Cyprinus carpio) – a first confirmed case report of protothecosis in a fish. J Fish Dis. 2017; 40(10): 1417–1421.
33.
Schöniger S, Roschanski N, Rösler U, et al. Prototheca species and Pithomyces chartarum as causative agents of rhinitis and/or sinusitis in horses. J Comp Pathol. 2016; 155: 121–125.
34.
Sapierzyński R, Jońska I, Ostrzeszewicz M. Obraz morfologiczny zapalenia nerek u zwierząt. Życie Wet. 2018; 93(10): 700–711.
35.
Whipple KM, Wellehan JF, Jeon AB, et al. Cytologic, histologic, microbiologic, and electron microscopic characterization of a canine Prototheca wickerhamii infection. Vet Clin Pathol. 2020; 49: 326–332.
36.
Huth N, Wenkel RF, Roschanski N, et al. Prototheca zopfii genotype 2-induced nasal dermatitis in a at. J Comp Pathol. 2015; 152(4): 287–290.
37.
Macedo JTSA, Riet-Correa F, Dantas AFM, et al. Cutaneous and nasal protothecosis in a goat. Vet Pathol. 2008; 45: 352–354.
38.
Malinowski E, Lassa H, Kłossowska A. Isolation of Prototheca zopfii from inflamed secretion of udders. Bull Vet Inst Pulawy. 2002; 46: 295–299.
39.
Bakuła Z, Ratajczyk A, Krukowski H, et al. Identyfikacja szczepów Prototheca izolowanych z przypadków mastitis od krów mlecznych z terenu Polski. Uniwersytet Warszawski, 2014.
40.
Jagielski T, Buzzini P, Lassa H, et al. Multicentre Etest evaluation of in vitro activity of conventional antifungal drugs against European bovine mastitis Prototheca spp. isolates. J Antimicrob Chemother. 2012; 67: 1945–1947.
41.
Wawron W, Bochniarz M, Piech T, et al. Outbreak of protothecal mastitis in a herd of dairy cows in Poland. Bull Vet Inst Pulawy. 2013; 57: 335–339.
42.
Tyczkowska-Sieron E, Markiewicz J, Grzesiak B, et al. Cold atmospheric plasma inactiva-tion of Prototheca zopfii isolated from bovine milk. J Dairy Sci. 2018; 10: 118–122.
43.
Jagielski T, Roeske K, Bakuła Z, et al. A survey on the incidence of Prototheca mastitis in dairy herds in Lublin province, Poland. J Dairy Sci. 2019; 102: 619–628.
44.
Shahid M, Cobo E R, Chen L, et al. Prototheca zopfii genotype II induces mitochondrial apoptosis in models of bovine mastitis. Sci Rep. 2020; 10, 698: 1–10.
45.
Shahid M, Cavalcante PA, Knight CG, et al. Murine and human cathelicidins contribute differently to hallmarks of mastitis induced by pathogenic Prototheca bovis glonae. Front Cell Infect Microbiol. 2020; 10: 31.
46.
Kwieciński J. Biofilm formation by pathogenic Prototheca glonae. Lett Appl Microbiol. 2015; 61: 511–517.
47.
Jagielski T, Krukowski H, Bochniarz M, et al. Prevalence of Prototheca spp. on dairy farms in Poland – a cross-country study. Microb Biotechnol. 2019; 12(3): 556–566.
48.
Grzesiak B, Krukowski H, Bis-Wencel H, et al. Wstępna ocena właściwości bójczych ekstraktu glicerynowo-wodnego z korzenia mydlnicy lekarskiej na szczepy glonów Prototheca zopfii. Post Mikrobiol. Suplement. 2019; 58(1): 112.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.