REVIEW PAPER
The impact of the Chernobyl nuclear power plant disaster on thyroid cancer – a review of recent reports
1
Southern Hospital, Warsaw, Poland
2
Ludwik Rydygier Specialist Hospital, Kraków, Poland
3
Student Scientific Club at the I Department of Psychiatry, Psychotherapy and Early Intervention, Medical University, Lublin, Poland
Corresponding author
Med Srod. 2024;27(1):1-6
KEYWORDS
TOPICS
Health effects of environmental pollutionEnvironmental toxicology (physical, chemical and biological factors)Health effects of social factors
ABSTRACT
Introduction and objective:
The Chernobyl nuclear power plant disaster in 1986 is one of the most tragic in human history. In addition to the immediate effects as a result of the release of many radioactive isotopes, the distant health consequences play a huge role. Their scale is enormous and, at the same time, very difficult to determine precisely. One of the most significant aspects associated with a reactor accident, is the risk of cancer, even many years after the incident itself. The aim of the review is an attempt to provide an insight into the Chernobyl nuclear reactor accident as a factor affecting thyroid cancer.
Brief description of the state of knowledge:
Most studies have consistently shown a significant effect of ionising radiation on the increased risk of thyroid cancer. Large amounts of radioisotopes released into the atmosphere have a well-documented effect on the occurrence of various thyroid gland cancers. In addition to methods of radiation absorption, such as inhalation of radionuclides, significant pathways of radiation exposure through the ingestion of contaminated milk or, for example, the effects of nitrates, have been described. The potential impact of radiation on thyroid tumours depends on the age group, gender and radiation dose received. Specific genetic mutations are also increasingly well studied and documented. Individual studies, however, cast doubt on the relevance of the correlation between the occurrence of thyroid cancer and the Chernobyl accident.
Summary:
In view of the huge population effect of the Chernobyl disaster, it seems justified to carry out a thorough analysis of its aftermath – including long-term effects. This will not only allow us to improve our knowledge of the impact of radiation on cancer, but also, perhaps, enable more effective prevention in the event of similar incidents in the future.
The Chernobyl nuclear power plant disaster in 1986 is one of the most tragic in human history. In addition to the immediate effects as a result of the release of many radioactive isotopes, the distant health consequences play a huge role. Their scale is enormous and, at the same time, very difficult to determine precisely. One of the most significant aspects associated with a reactor accident, is the risk of cancer, even many years after the incident itself. The aim of the review is an attempt to provide an insight into the Chernobyl nuclear reactor accident as a factor affecting thyroid cancer.
Brief description of the state of knowledge:
Most studies have consistently shown a significant effect of ionising radiation on the increased risk of thyroid cancer. Large amounts of radioisotopes released into the atmosphere have a well-documented effect on the occurrence of various thyroid gland cancers. In addition to methods of radiation absorption, such as inhalation of radionuclides, significant pathways of radiation exposure through the ingestion of contaminated milk or, for example, the effects of nitrates, have been described. The potential impact of radiation on thyroid tumours depends on the age group, gender and radiation dose received. Specific genetic mutations are also increasingly well studied and documented. Individual studies, however, cast doubt on the relevance of the correlation between the occurrence of thyroid cancer and the Chernobyl accident.
Summary:
In view of the huge population effect of the Chernobyl disaster, it seems justified to carry out a thorough analysis of its aftermath – including long-term effects. This will not only allow us to improve our knowledge of the impact of radiation on cancer, but also, perhaps, enable more effective prevention in the event of similar incidents in the future.
REFERENCES (26)
1.
Mousseau TA. The biology of Chernobyl. Ann Rev Ecol Evol System. 2021;52(1):87–109. doi:10.1146/annurev-ecolsys-110218-024827.
2.
Albi E, Cataldi S, Lazzarini A, Codini M, Beccari T, Ambesi-Impiombato FS, Curcio F. Radiation and Thyroid Cancer. Int J Mol Sci. 2017;18(5):911. doi:10.3390/ijms18050911.
3.
Takamura N, Yamashita S. Lessons from Chernobyl. Fukushima J Med Sci. 2011;57(2):81–85. doi:10.5387/fms.57.81.
4.
Thomas G. Radiation and thyroid cancer-an overview. Radiat Prot Dosimetry. 2018;182(1):53–57. doi:10.1093/rpd/ncy146.
5.
Nabhan F, Dedhia PH, Ringel MD. Thyroid cancer, recent advances in diagnosis and therapy. Inter J Cancer. 2021 Sep;149(5):984–992. doi:10.1002/ijc.33690. PMID: 34013533.
6.
Chmielik E, Rusinek D, Oczko-Wojciechowska M, et al. Heterogeneity of Thyroid Cancer. Pathobiol. 2018;85(1–2):117–129. doi:10.1159/000486422.
7.
Tanja M, Olivija V, Sinisha S, Nevena M, Daniela M, Vesna VS. Epidemiology of Thyroid Carcinomas in North Macedonia (1999–2015). J Prim Care Community Health. 2021;12:21501327211004286. doi:10.1177/21501327211004286.
8.
Carling T, Udelsman R. Thyroid cancer. Annu Rev Med. 2014;65:125–137. doi:10.1146/annurev-med-061512-105739.
9.
Kumar R, De Jesus O. Radiation Effects On The Fetus. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 23, 2023.
10.
Kutkov V, Buglova E, McKenna T. Severe deterministic effects of external exposure and intake of radioactive material: basis for emergency response criteria. J Radiol Prot. 2011;31(2):237–253. doi:10.1088/0952-4746/31/2/003.
11.
Imanaka T, Hayashi G, Endo S. Comparison of the accident process, radioactivity release and ground contamination between Chernobyl and Fukushima. J Radiat Res. 2015;56 doi:10.1093/jrr/rrv074.
12.
Stosic, Zoran V, Werner B, Uwe S. Boiling water reactor with innovative safety concept: The Generation III+ SWR-1000. Nucl Engin Design. 2008;238:1863–1901.
13.
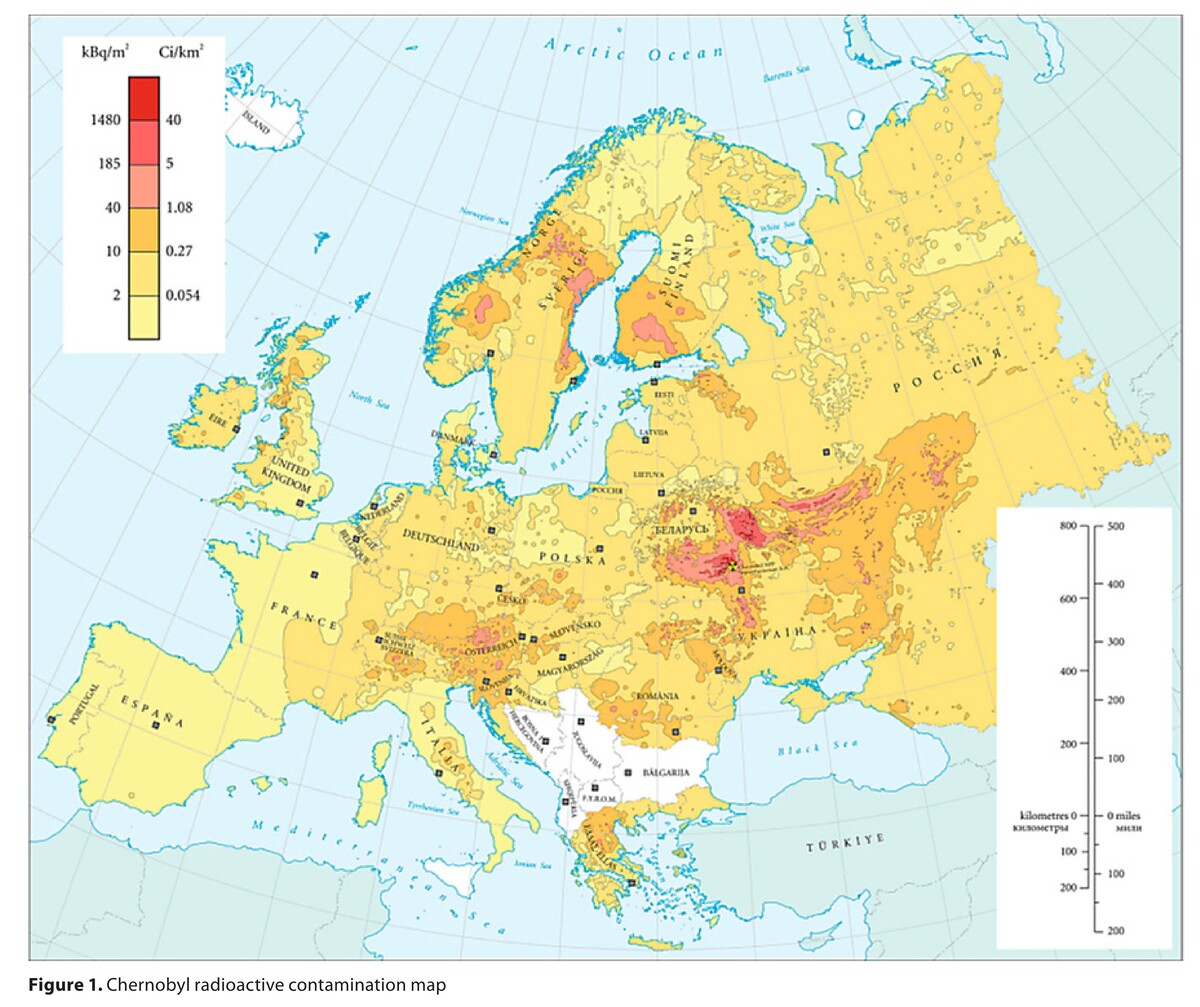
Marino F, Nunziata L. Long-Term Consequences of the Chernobyl Radioactive Fallout: An Exploration of the Aggregate Data. Milbank Q. 2018;96(4):814–857. doi:10.1111/1468-0009.12358.
14.
Smailyte G, Kaceniene A, Steponaviciene R, Kesminiene A. Lithuanian cohort of Chernobyl cleanup workers: Cancer incidence follow-up 1986–2012.Cancer Epidemiol. 2021;74:102015. doi:10.1016/j.canep.2021.102015.
15.
Drozdovitch V. Radiation Exposure to the Thyroid After the Chernobyl Accident. Front Endocrinol (Lausanne). 2021;11:569041. Published 2021 Jan 5. doi:10.3389/fendo.2020.569041.
16.
Weiss W. Chernobyl thyroid cancer: 30 years of follow-up overview. Radiat Prot Dosimetry. 2018;182(1):58–61. doi:10.1093/rpd/ncy147.
17.
Efanov AA, Brenner AV, Bogdanova TI, et al. Investigation of the Relationship Between Radiation Dose and Gene Mutations and Fusions in Post-Chernobyl Thyroid Cancer [published correction appears in J Natl Cancer Inst. 2018 Jun 1;110(6):685]. J Natl Cancer Inst. 2018;110(4):371–378. doi:10.1093/jnci/djx209.
18.
Hatch M, Cardis E. Somatic health effects of Chernobyl: 30 years on. Eur J Epidemiol. 2017;32(12):1047–1054. doi:10.1007/s10654-017-0303-6.
19.
Takamura N, Orita M, Saenko V, Yamashita S, Nagataki S, Demidchik Y. Radiation and risk of thyroid cancer: Fukushima and Chernobyl. Lancet Diabetes Endocrinol. 2016;4(8):647. doi:10.1016/S2213-8587(16)30112-7.
20.
Fisher SB, Cote GJ, Bui-Griffith JH, et al. Genetic characterization of medullary thyroid cancer in childhood survivors of the Chernobyl accident. Surgery. 2019;165(1):58–63. doi:10.1016/j.surg.2018.08.029.
21.
Fridman M, Krasko O, Branovan DI, et al. Factors affecting the approaches and complications of surgery in childhood papillary thyroid carcinomas. Eur J Surg Oncol. 2019;45(11):2078–2085. doi:10.1016/j.ejso.2019.07.032.
22.
Drozd VM, Branovan I, Shiglik N, Biko J, Reiners C. Thyroid Cancer Induction: Nitrates as Independent Risk Factors or Risk Modulators after Radiation Exposure, with a Focus on the Chernobyl Accident. Eur Thyroid J. 2018;7(2):67–74. doi:10.1159/000485971.
23.
Drozd V, Saenko V, Branovan DI, Brown K, Yamashita S, Reiners C. A Search for Causes of Rising Incidence of Differentiated Thyroid Cancer in Children and Adolescents after Chernobyl and Fukushima: Comparison of the Clinical Features and Their Relevance for Treatment and Prognosis. Int J Environ Res Public Health. 2021;18(7):3444. Published 2021 Mar 26. doi:10.3390/ijerph18073444.
24.
Oliynyk O, Slifirchik A, Potupalova T, Slobodian V. Sickness rate and prevalence of thyroid cancer in a specific region of Ukraine 30 years after Chernobyl disaster. Health Prob Civil. 2018;12(1):29–32.
25.
Jargin SV. Chernobyl-related thyroid cancer. Eur J Epidemiol. 2018;33(4):429–431. doi:10.1007/s10654-018-0391-y.
26.
Jargin S. Thyroid Cancer After Chernobyl: Re-Evaluation Needed. Thyroid Cancer After Chernobyl: Re-Evaluation Needed. Turk Patoloji Derg. 2021;37(1):1–6. doi:10.5146/tjpath.2020.01489.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.